Using the Competencies for Canada’s Substance Use Workforce is an evidence-informed way to ensure services are provided consistently across the wide range of backgrounds and settings in the substance use field, including among both regulated and unregulated professionals who support this work.
To maximize the benefits of the Competencies for Canada’s Substance Use Workforce to an organization that delivers substance use services and the people who seek those services, the organization must understand exactly what the competencies are and how they can be of assistance.
The information in the tabs below will help you understand how the competencies can benefit your organization and the people it serves.
You will find learning about:
- Why workforce competencies are needed;
- Who should use the competencies;
- How to use the competencies;
- The difference between behavioural and technical competencies;
- The skills and knowledge required for a range of job functions;
- The four levels of proficiency for the competencies and how they are defined; and
- A glossary of important terms related to the competencies.
Having this knowledge will prepare you for using the Competencies for Canada’s Substance Use Workforce to help your organization provide professional and consistent services to its clients.
Secondary Body
What You
Need to Know
What You Need to Know
CCSA identified Technical and Behavioural Competencies for Canada’s Substance Use Workforce across four levels of proficiency.
The knowledge and skills or the “what“ of a job; sometimes called “hard” skills. Usually learned through education and experience.
The knowledge, skills and values or the “how” of performing a job. Typically learned and developed through life experiences and coaching by mentors.
Levels of Proficiency
Different jobs require competencies at different levels of proficiency. The proficiency levels are cumulative. For example, someone who is required to have a Developing (or Level 2) proficiency is also expected to have the Foundational (or Level 1) proficiency.
The four proficiency levels and how the knowledge and skills for them are typically developed are described in the following table. In the table, “life experience” can mean direct, lived and living experience with substance use, mental health concerns or concurrent conditions, or experience as someone close to another with direct experience of substance use, mental health concerns or concurrent conditions.
Explanation of Proficiency Levels
| Proficiency Level |
Explanation of Level |
How Knowledge and Skills Are Typically Developed for the Level |
|---|---|---|
| Level 1 Foundational | Demonstrates basic knowledge and ability, and can apply the competency, with guidance, in common situations that present no or limited difficulties. | Through student practicum, entry level work experience, volunteering, in-service training, introductory-level college or university courses; completion of a diploma or certificate, possibly combined with life experience. |
| Level 2 Developing | Demonstrates sound knowledge and ability, and can practically apply the competency and associated knowledge and skills, with minimal or no guidance, in the full range of typical situations. Likely requires guidance to handle novel or more complex situations. | Through work experience at Level 1, completion of a college diploma or university degree in health or social services, participation in a mentoring program, in-service training, possibly combined with life experience. |
| Level 3 Proficient | Demonstrates in-depth knowledge and ability, and can consistently and effectively apply the competency in complex and challenging situations and settings. Guides other professionals. | Through the completion of a university degree in mental health or substance use studies and several years of work experience; a university degree in health or social services combined with professional development and work experience; a diploma or certificate in substance use, mental health or other health or social services area, professional development and in-service training, possibly combined with life experience. |
| Level 4 Advanced | Demonstrates expert knowledge and ability and can apply the competency in the most complex situations. Develops or facilitates new practices, programs and policies. Is recognized as an expert, internally and externally. Involved in leadership and decision-making processes, as applicable. | Through comprehensive work experience or completion of a related graduate or undergraduate university degree, combined with extensive work experience; a diploma or certificate, combined with extensive and demonstrated professional development, in-service training and extensive work experience, possibly combined with life experience. |
Behaviour Indicators
Behaviour indicators are examples of a person’s successful performance at each level of proficiency. These indicators are neither exhaustive nor mandatory, but provide guidance and illustration.
The language used to describe these indicators might not be wholly applicable to your organization and you might want to add other relevant indicators. It is important to review the sample behaviour indicators and modify them accordingly before applying them to positions in your organization.
Example of Behaviour Indicators for Adaptability and Flexibility
| Foundational (Level 1) | Developing (Level 2) | Proficient (Level 3) | Advanced (Level 4) |
|---|---|---|---|
| Readily shows flexibility and expresses willingness to do things differently, accepting change as normal. | Remains effective and retains perspective under changing or unclear conditions. | Provides advice and guidance to others to assist them in adapting to difficult or changing situations. | Provides support systems (e.g., retraining programs) to deal with the unanticipated and challenging results of change activities. |
Why We Need
Competencies
Why We Need Competencies
Using competencies is an evidence-based way to bring consistency to similar roles across a wide range of practices, contexts and settings in the substance use field.
The backgrounds of people working in the substance use field vary widely, from academically trained direct service providers, such as addictions counsellors, social workers and nurses, to other roles, such as volunteers or Elders. Care settings also vary widely and can include accredited hospitals and residential treatment centres, community settings for support groups, withdrawal management centres, private care centres and supervised consumption sites.
A competency-based approach to workforce development in the substance use field enhances professionalism and consistency of practice by:
- Identifying knowledge and skill sets for the substance use workforce and allied professionals;
- Supporting employers in hiring, retaining and developing staff;
- Assisting educators and trainers in developing content for learning;
- Facilitating role definition and collaboration in multi-disciplinary teams; and
- Providing Canadians with a more consistent quality of service from the substance use workforce.
Who Should Use
the Competencies
Who Should Use the Competencies
The Technical and Behavioural Competencies for Canada’s Substance Use Workforce are useful for people working in a range of roles in the field of substance use.
Roles for which Competencies Are Useful
Direct Service Professionals
- Outreach service providers in harm reduction and drug use prevention programs
- Clinicians and supervisors in treatment programs
- Nursing staff in substance use programs and services
- Health promotion staff
- Counsellors
- Technicians
Medical and Allied Professionals
- Primary healthcare providers
- Doctors and physicians
- Specialist practitioners (physicians or nurses trained in mental health and substance use)
- Pharmacists
- Dentists
- Nurses and nurse practitioners
- Family practice nurses
- Midwives
- Occupational therapists
- Physiotherapists
- Public health nurses
- Social workers
- Mental health service providers
- Housing service providers
- School guidance counsellors
- Emergency service providers
Administrators or Leadership Staff
- Office staff
- Program coordinators
- Supervisors
- Managers and senior managers
- Executive directors
- Human resources staff
- Recruiters
Educators
- Academics
- Educators
- Learning and development staff
Researchers
- Policy analysts
- Policy advisors
- Researchers
How the
Competencies
Are Used
How the Competencies Are Used
The Technical and Behavioural Competencies for Canada’s Substance Use Workforce are intended to be used as a guide and are not prescriptive. They may be tailored to different job descriptions, work settings and organizational cultures.
The Competencies can be used for a variety of purposes, including:
- Developing and refining job profiles;
- Interviewing and assessing suitability of candidates for positions;
- Developing competency-based education and training curricula;
- Evaluating job performance;
- Identifying and self-assessing professional development needs; and
- Clarifying succession planning requirements.
The Competencies are intended to be used by certification and regulatory bodies in conjunction with complementary standards and federal, provincial and territorial requirements. They are not meant to replace clinical regulations or best practice guidelines.
Competencies
Video Series
Competencies Video Series
The substance use field continues to evolve quickly. Skill sets and knowledge requirements for staff are continually changing and finding qualified professionals to meet growing needs is essential.
CCSA's Behavioural and Technical Competencies for Canada’s Substance Use Workforce describe the behaviours, skill sets and knowledge required for regulated and unregulated professionals who work with people who use substances.
We have created three training videos to support you in applying the Competencies. The Competencies for Canada’s Substance Use Workforce video series guides you through how to use the Competencies in practice.
Video 1: Overview
This video provides an overview of how a competency-based framework using the Behavioural and Technical Competencies for Canada’s Substance Use Workforce can help your organization.
Video 2: Job Descriptions and Roles
This video describes how to clarify job descriptions and roles using the Competencies for Canada’s Substance Use Workforce.
Video 3: Interviewing and Performance Management
This video describes how to use the interviewing and performance management tools to support the application of the Competencies for Canada’s Substance Use Workforce.
History
Acknowledgements
History Acknowledgements
The Technical and Behavioural Competencies for Canada’s Substance Use Workforce were developed with the involvement of a wide range of stakeholders. Extensive consultation was a priority to ensure the competencies were informed by evidence from researchers and experts, and grounded in the realities of people working in the substance use field and people with lived and living experience of substance use and their families and friends.
Input was gained from:
- Direct treatment service and program delivery staff
- Allied professions in the field such as nurses and probation officers
- People with lived and living experience of substance use and their families and friends
- Provincial and territorial departments of health
- Key national organizations focused on substance use and mental health
- Expert review panels
- Mental health workers
A variety of formats were used to engage stakeholders, including focus groups, informant interviews, and teleconferences with groups and blog contributors.
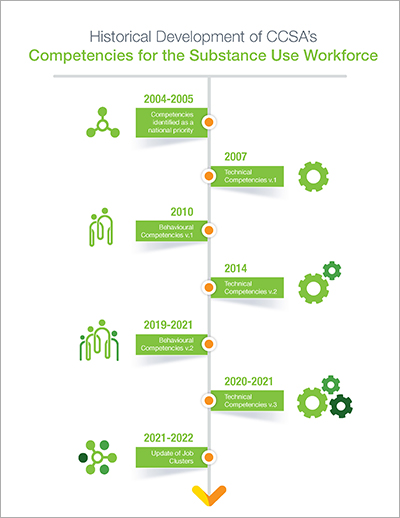
Updates to the Competencies
A culture shift in the substance use field is occurring due to the recognition of the neurobiological underpinnings of substance use disorders and the harmful impact of stigma around substance use. We responded to this shift by updating the Competencies (version 2) through more community consultations and with input from subject-matter experts, advisory groups and people with lived and living experience and their families and friends to reflect changes in best practices, knowledge, skills and language, and to apply a perspective oriented to well-being.
An overview of the development of the Competencies provides more detail.
Historical Development Timeline
Click image below to see the historical development timeline of
CCSA’s competencies for the substance use workforce.
Acknowledgements
The Canadian Centre on Substance Use and Addiction (CCSA) gratefully acknowledges the significant contributions and support received from individuals, subject-matter experts and CCSA’s workforce competencies advisory group members who participated in interviews, focus groups and consultations across Canada to update the Technical and Behavioural Competencies for Canada’s Substance Use Workforce.
We also thank the Lived and Living Experience and Families and Friends (LLEAFF) Working Group and sub-committee who participated in the revision and development of new and revised competencies through their valuable feedback and diverse expertise.
We acknowledge members of the historical National Advisory Group on Workforce Development and Knowledge Exchange Network on Workforce Development who participated in the original reviews of both the Technical and Behavioural Competencies. Special thanks to the Mental Health Commission of Canada which participated in the review of the concurrent disorders competency and with which we continue to work to identify needs for integrated substance use and mental health competencies.
We also acknowledge Kiran Somjee, RN, Knowledge Broker, Claire Rykelyk-Huizen, RSW, MSW, Knowledge Broker, Cheryl Arratoon, MSc, as well as CCSA’s Information Systems and Web Services and Public Affairs and Communications teams for their contributions in revising, publishing, disseminating and mobilizing the competencies. We would like to thank our contractors, the Human Resources Services Group and the Industrial design agency, for their involvement on this project.
It is only with the valuable feedback, participation and strategic recommendations from those above that the Technical and Behavioural Competencies for Canada’s Substance Use Workforce could be updated.
Glossary
Glossary
This glossary provides definitions of key terms used in the Technical and Behavioural Competencies for Canada’s Substance Use Workforce. The definitions reflect the environment and context in which professionals working with people who use substances deliver services.
ACEs (Adverse Childhood Experiences)
Adverse Childhood Experiences (ACEs) are “negative, stressful, traumatizing events that occur before the age of 18 and confer health risks across the lifespan” (Alberta Family Wellness, 2020; retrieved from https://www.albertafamilywellness.org/what-we-know/aces). Examples of ACEs include physical or emotional abuse or neglect, sexual abuse and household dysfunction. The more ACEs experienced, the greater the chance of poor outcomes later in life, including increased risk of substance use and mental health conditions, such as depression.
Assessment (see also Screening)
In-depth, ongoing process to inform the therapeutic approach. The practitioner collaborates with the individual and in consultation with them establishes the presence or absence of a challenge, identifies strengths and barriers to engagement, and areas of resilience, and determines whether there is a need for crisis intervention or specialist practitioner support, intervention or treatment.
Concurrent Substance Use and Mental Health Conditions
A combination or co-occurrence of a substance use condition and a mental health condition Examples of concurrent substance use and mental health conditions are:
- Harmful use of alcohol and an anxiety disorder
- Cannabis dependence and schizophrenia
- Heroin dependence and borderline personality disorder
Evidence-informed
Service approaches guided by the best available research and practice-based knowledge including traditional knowledge for culturally appropriate services. Evidence-informed service approaches allow for innovation while incorporating lessons learned from existing research literature and being responsive to cultural backgrounds, community values and individual preferences. Evidence-based practices are practices validated by some form of documented scientific evidence.
Family (see also Social Support)
Persons or groups who constitute family both in the traditional sense and in a broader sense that includes any configuration of significant others in the past, present or future of the individual who is seeking well being, who can either support or influence the individual’s well being goals. These significant others can include spouses, partners, children, parents, siblings, friends, Elders or other people active in the individual’s social support system.
Knowledge
Awareness, information or understanding about facts, rules, principles, guidelines, concepts, theories and processes needed to perform a task successfully.
Mental Health
A continuum of psychological and emotional well-being along which an individual moves periodically without having a mental illness. The World Health Organization defines mental health as a state of well-being in which an individual realizes their own potential, can cope with the normal stresses of life, can work productively and fruitfully, and is able to make a contribution to their community.
Mental Illness
Psychiatric disorder or mental-health impairment, diagnosed by a specialist practitioner, that requires treatment, often including medication. Refer to Diagnostic and Statistical Manual of Mental Disorders (5th edition, DSM-5).
People
People may include individuals, families, friends, groups, communities and organizations.
People Affected by Substance Use
Individuals, families, friends, groups, communities or organizations seeking assistance and support to reduce the harms of substance use and achieve well-being as they define it.
People with Lived or Living Experience
People with lived and living experience refers to people who have used or are using one or more substance.
Recovery
Recovery is a dynamic process towards well-being that is free of stigma and discrimination and is unique to individual strengths, cultures and experiences. Recovery is supported by collaboration among services across many levels, including communities, sectors and systems. It extends beyond the individual and involves family, peers and workplaces. Recovery is multidimensional, involving all aspects of physical, social, mental, emotional and spiritual health.
Screening (see also Assessment)
Brief initial process using screening tools to consult with an individual about their substance use and any concerns they may have about it.
Self Care
Deliberately and continuously take action at a professional and personal level to protect and preserve one’s own well-being, especially during times of stress.
Social Support (see also Family)
Individuals or groups who constitute social networks, Elders, community systems and any configuration of significant others in the individual’s past, present or future, and who can either support or undermine the individual’s wellness goals.
Specialist Practitioner
Psychiatrists, psychologists and other regulated clinicians trained in substance use and mental health who can diagnose and treat substance use and mental health conditions.
Substance Use
The self-administration of a psychoactive substance. For CCSA’s Competencies, substance use is inclusive of situations where professionals are working with individuals who use or have used substances, are diagnosed with a substance use disorder or are experiencing harms as a result of using substances. Refer to the criteria for substance use disorders in the Diagnostic and Statistical Manual of Mental Disorders (5th edition, DSM-5).
Trauma
Experiences that overwhelm an individual’s capacity to cope. Such experiences include trauma early in life (e.g., child abuse and neglect, witnessing violence) and later traumatic experiences (e.g., accidents, war, natural disasters). See also ACEs and Trauma- and Violence-informed Care.
Trauma- and Violence-informed Care
“Trauma and violence informed approaches are policies and practices that recognize the connections between violence, trauma, negative health outcomes and behaviours. These approaches increase safety, control and resilience for people who are seeking services in relation to experiences of violence and/or have a history of experiencing violence” (Government of Canada, 2018; retrieved from https://www.canada.ca/en/public-health/services/publications/health-risks-safety/trauma-violence-informed-approaches-policy-practice.html).
Skill
The capacity to perform mental or physical tasks with a specific job outcome. As with knowledge, skills can range from highly concrete and easily identifiable tasks, such as completing a checklist during an assessment interview, to less tangible and more abstract tasks, such as managing community participation. Skills help determine whether a person’s training and experience have prepared them for a specific workplace activity.
Values
Concepts that determine the importance of emotion, orient choice or propel action. They are principles, beliefs or criteria for selecting what is good (or better or best), meaningful or right among objects, actions, ways of life, and social and political institutions and structures. Values operate at the level of individuals, of institutions and of entire societies.
Well-being
Well-being may be defined as the experience of health, happiness and life satisfaction. It will appear differently from one individual to another, with each having their own definition of what well-being means to them. Well-being can encompass a range of indicators, including physical, emotional and mental health, meaning and purpose in life, connections with others, and the ability to manage stress.